Checked: 23-08-2020 by
Vicky Ryan Next Review: 23-08-2021
Overview
Also consider checking the following specific pages:
Access to the most appropriate diagnostics from primary care should be encouraged where this facilitates the patient being cared for in primary care. This guidance has been compiled by the BNSSG planned care diagnostics team alongside primary and secondary care MSK clinicians. We welcome any feedback regarding the guidance, via the Remedy Feedback button (above right)
Guidance indicates the recommended appropriate diagnostic testing for back, shoulder, knees, small joint, soft tissue "swellings", brain and sinus. The intention is to provide advice and guidance in order to help GPs reduce the occurrence of unnecessary or inappropriate direct access referral for imaging.
To facilitate appropriate referrals to radiology departments, The Royal College of Radiologists (RCR) has published RCR iRefer Guidelines. Unfortunately, a charge has been introduced to access the guidelines so you cannot access these unless you subscribe.
Xrays not routinely performed
Recent advice from NBT radiology has listed a number of X-rays that are not routinely performed (in alignment with irefer guidelines):
- Nasal bone - X-rays are unreliable in the diagnosis of uncomplicated nasal fractures.
- Calcaneus for calcaneal spur/ plantar fasciitis/heel pain - Most patients with heel pain can be managed on the basis of clinical findings without imaging. Calcaneal spurs are common incidental findings. The cause of pain is rarely detectable on X-ray.
- Coccyx for trauma or coccydynia - Normal appearances on X-ray are often misleading and do not affect management and is considered to be significant radiation dose.
- Temporomandibular joint for pain or dysfunction - X-ray cannot detect common disc and soft tissue abnormalities.
- Skull for headache or trauma - Skull X-ray has no role in assessing head injury.
- Sinuses for sinusitis or headache - Signs on X-ray sinus are often non-specific and are encountered in asymptomatic people.
- Chest for rib fracture and no suspected complication e.g pneumothrorax - Patients with minor chest trauma and normal physical examination rarely require imaging.
- Abdominal x-rays unless for specific conditions (see Abdominal imaging section below)
If x-ray is requested for the above then it may be declined unless clear clinical reasons are given in the request.
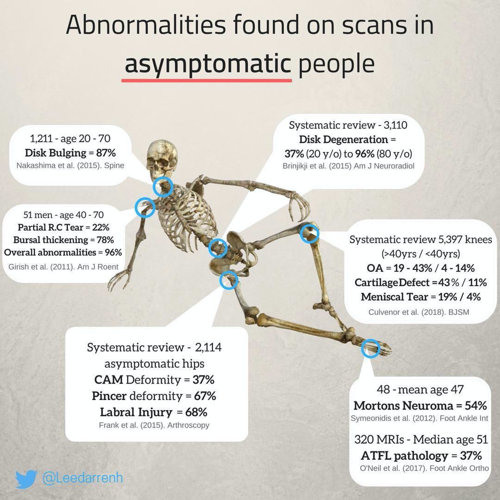
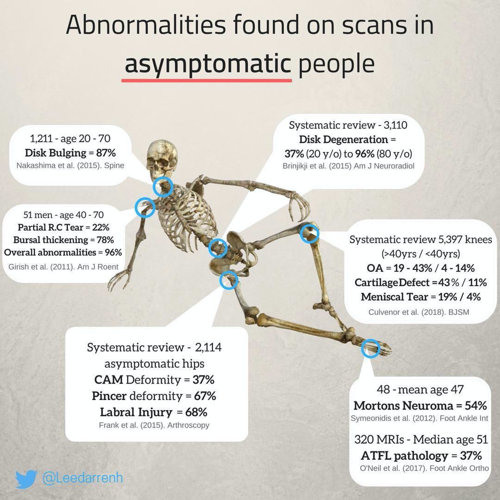
Diagram courtesy of Lee Higginbotham
Spine (Lumbar, Cervical, Thoracic)
Shoulders
- Plain film may be helpful in distinguishing frozen shoulder and osteoarthritis, and can demonstrate calcific tendinitis (please see the Shoulder Problems section of Remedy for guidance on the diagnosis of shoulder problems in primary care)
- Shoulder injection may be given without imaging control. Ultrasound is indicated where there is a diagnostic dilemma or failure to respond to first line treatment and where care is likely to be maintained in primary care. If you are considering a scan you should request a plain film at the same time
- MRI shoulder is usually for pre-operative planning and is not indicated from primary care unless discussed with a radiologist
Hips
- Plain film is less useful in the management of osteoarthritic hip pain unless there are clinical reasons to contemplate surgery. Arthritis is common in patients over 45. Please check there has been no previous similar imaging within the last 2 years. Plain film may demonstrate features associated with femoroacetabular impingement and dysplasia
- Consider referral to the emergency department if severe hip pain and sudden inability to weight bear +/- history of fall, sudden severe significant deterioration of chronic hip pain, sudden change in true leg length, suspected avascular necrosis or sepsis
Knees
- Please see the Knee pain page or Remedy which includes advice on imaging
- Plain film is less useful in the management of osteoarthritic knee pain unless there are clinical reasons to contemplate surgery. Arthritis is common in patients over 45. Please check there has been no previous similar imaging within the last 2 years
- MRI knee to rule out ligamentous or meniscal damage where urgent referral not indicated. Use plain film to rule out osteoarthritis as primary cause of symptoms in older patients. MRI does not add value in the investigation of the osteoarthritic knee. Surgery is unlikely to be contemplated unless there is significant osteoarthritis or true locking that fails to improve after 3 months of conservative management
- Ultrasound is only of value in assessment of quadriceps inflammation or tears and to assess the infra-patellar tendon
- Imaging of a Baker’s cyst is unnecessary
Previous Joint Replacement
- Plain film may demonstrate loosening of the prosthesis. Pain after metal-on-metal joint replacement requires investigation & referral to MSK services
Heel, Achilles and Foot
- Most cases can be diagnosed and managed using the clinical history and examination including plantar fasciitis, achilles tendinitis (including hagland’s deformity and heal spurring), and metatarsalgia (morton’s neuroma). Plain films of ankle and foot are required for those patients requiring surgical review
Soft tissue swellings
- Ultrasound is the investigation of choice. Referral should only be performed in situations of a diagnostic dilemma and should have a clear rationale documented in the referral. Avoid imaging of characteristic lipomas and ganglia. Lumps and bumps; to scan or not to scan...
- Consider 2 week wait sarcoma referral for:
- suspicious soft tissue mass >5cm diameter
- Any deep, hard, fixed mass
- Any enlarging or painful soft tissue mass
Brain
- CT scan is the initial investigation of choice.
- Requests for MRI should be discussed with radiology – guidelines to be developed
- Brain imaging for patients with headache: see the Headache section of Remedy for advice on 'Who should be investigated for brain tumour in primary care'
- Also see the Brain and CNS suspected cancer section for advice on appropriate 2WW referral.
Sinus
- Imaging rarely adds value.
- MRI and CT not available to primary care and is for pre operative planning procedures.
USS guided steroid injections
See the Image guided steroid injection page
Abdominal imaging
Abdominal x-ray requests - advice from NBT radiology
Abdominal X rays are not routinely performed. Abdominal X ray requests will only be accepted for the following clinical indications.
- Bowel obstruction - clinical suspicion of large bowel obstruction
- Overflow diarrhoea - on inpatients with diarrhoea suspected to be due to faecal impaction
- Foreign bodies or renal calculi- to document renal calculus and foreign body position, including stents, catheters, and other devices
- Flare of IBD - to check for toxic dilatation in known inflammatory bowel disease
Any other indication will be rejected.
USS abdo requests
Requests for abdo USS should provide sufficient clinical information. Requests for vague abdominal symptoms may be rejected or redirected to CT or MRI. See USS guidance for further details.
Resources
COVID-19 Update: Please see below updates regarding Radiology Services
Efforts are made to ensure the accuracy and agreement of these guidelines, including any content uploaded, referred to or linked to from the system. However, BNSSG ICB cannot guarantee this. This guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer, in accordance with the mental capacity act, and informed by the summary of product characteristics of any drugs they are considering. Practitioners are required to perform their duties in accordance with the law and their regulators and nothing in this guidance should be interpreted in a way that would be inconsistent with compliance with those duties.
Information provided through Remedy is continually updated so please be aware any printed copies may quickly become out of date.