

This page is for children aged 12 months to 16 years with acute wheeze/ asthma. This includes children with an established diagnosis of asthma, first presentations of asthma, and wheezing during viral infections in preschool-aged children.
In all cases, an acute wheeze attack signals a risk for future attacks and this risk should be assessed and managed as well as the acute episode.
Please refer to the guidelines below:
See also the Asthma in Children - Chronic page.
For children aged less than 12 months then wheezing is usually associated with bronchiolitis and does not respond to treatment with steroids. Please see the Bronchiolitis page for details.
For adults aged 16 and over see the Asthma (adults) page.
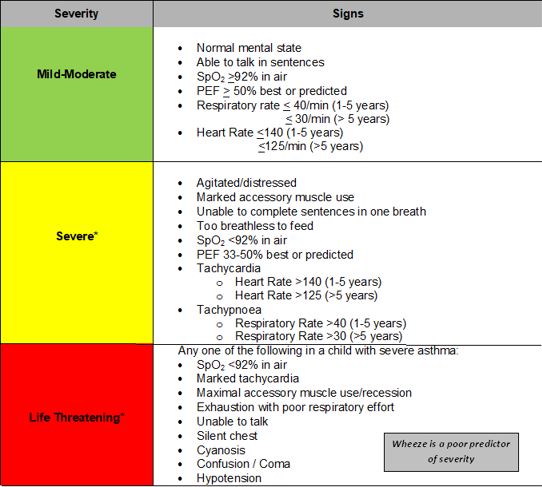
Assessment of acute wheeze/asthma:
Management in Primary Care
In children with mild-moderate wheeze/asthma give up to 10 puffs of Salbutamol by MDI + spacer & assess response (in < 5 years: 5-10 puffs, 1 puff per minute)
See assessment section above for advice on red flag signs and symptoms.
Children who have a severe episode of wheeze/asthma or who are not responding to treatment in primary care should be admitted to the Children's ED, or if unsure if admission is required then discuss with the ED helpline: Children's Urgent Care Referrals
Children with severe or life-threatening wheeze/asthma should be treated with salbutamol nebulisers and prednisolone (if possible) whilst arranging emergency transfer to CED. Call the CED team on 0117 3428666 for guidance on acute management whilst awaiting an ambulance.
BTS/SIGN guidelines on the management of asthma - 2019 - page has links to full guideline and quick guideline.
CKS guidelines on Asthma (all ages) - May 2021
BNSSG Asthma Prescribing guidelines for children are available in the Formulary Local Guidance section of Remedy.
Efforts are made to ensure the accuracy and agreement of these guidelines, including any content uploaded, referred to or linked to from the system. However, BNSSG ICB cannot guarantee this. This guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer, in accordance with the mental capacity act, and informed by the summary of product characteristics of any drugs they are considering. Practitioners are required to perform their duties in accordance with the law and their regulators and nothing in this guidance should be interpreted in a way that would be inconsistent with compliance with those duties.
Information provided through Remedy is continually updated so please be aware any printed copies may quickly become out of date.