Checked: 11-02-2025 by
Jenny Henry Next Review: 11-02-2027
Overview
Definition
- A condition in which the adrenal glands produce inadequate levels of steroid hormones; primarily cortisol, but also mineralocorticoids (aldosterone) and androgens. It is classified as:
- Primary (adrenal in origin) – most commonly autoimmune e.g. Addison’s disease (80-90% of cases).
- Secondary (due to pituitary dysfunction/destruction) including following prolonged exogenous steroid use.
- Tertiary (due to hypothalamic dysfunction/destruction) including following prolonged exogenous steroid use.
- The most common cause of adrenal insufficiency is the sudden withdrawal of long-term exogenous steroids.
When to suspect adrenal insufficiency
- Adrenal insufficiency can present acutely (a medical emergency – see red flags below) or chronically (often an insidious presentation)
- Consider adrenal insufficiency when there is no other clinical explanation for the presence of one or more of the following persistent symptoms:
- Fatigue or muscle weakness
- Weight loss
- Hyperpigmentation (primary)
- Dizziness or hypotension
- Salt craving
- Gastrointestinal symptoms – anorexia, nausea, vomiting, diarrhoea or abdominal pain
- Unexplained hypoglycaemia (including in those with Type 1 Diabetes - a marked reduction in insulin requirements may be the first sign)
- Unexplained hyponatraemia or hyperkalaemia
- Also consider the diagnosis of adrenal insufficiency in the following circumstances:
- Personal or family history of autoimmune disease
- Anyone with the above symptoms who have recently stopped using high dose steroids (by any route), after taking them for more than 4 weeks
- Anyone taking glucocorticoids at physiological equivalent doses or above (by any route) and have had an episode of physiological stress
- Anyone taking certain medications including long-term high dose opiates, immunotherapy/checkpoint inhibitors for cancer, adrenal enzyme inhibitors e.g. fluconazole
Red Flags
An adrenal crisis is a MEDICAL EMERGENCY. If left untreated, it can lead to coma and death. Where the patient shows signs of acute adrenal crisis, no further investigation is required.
Signs of an adrenal crisis include:
- Severe dehydration
- Clinical shock - pale, cold, clammy skin, tachycardia, low blood pressure
- Sweating
- Severe vomiting and diarrhoea
- Severe muscle weakness
- Hypoglycaemia
- Headache
- Drowsiness/decreased level of consciousness
If you think a patient is having an adrenal crisis:
- Dial 999 for an ambulance
- Give 100mg intravenous (IV) or intramuscular (IM) hydrocortisone immediately (the intramuscular dose can be given by anyone, including self-administration using an emergency management kit)
- Further information regarding how to give an IM hydrocortisone injection can be on the Addison’s Disease website: Adrenal Crisis Emergency Injection Guidance | Addison's Disease Self Help Group
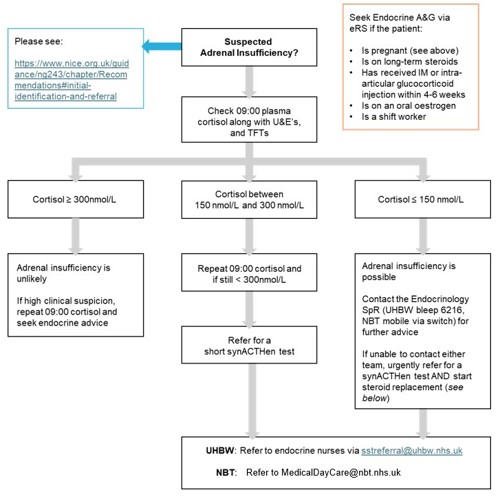
Investigation of Suspected Adrenal Insufficiency
The following clinical evaluation and investigation in primary care can be considered, including but not limited to:
- U&Es – this occasionally demonstrates a low sodium and/or high potassium (but often the result is normal)
- 09:00 serum cortisol, glucose, TFTs (see below for interpretation)
- Be aware of people taking exogenous steroids by non-oral routes (e.g. inhaled, intramuscular, topical)
- Ideally omit all steroids for 24 hours before a cortisol measurement (or synACTHen test)
- Please inform the lab (via the ICE request) if the patient is taking an oral oestrogen e.g. the COCP/HRT or if they are pregnant
- Do not test for adrenal insufficiency in people taking oral glucocorticoids above physiological equivalent dose (>4mg Prednisolone/day OR hydrocortisone 20mg daily)
- Consider a full 9am pituitary panel in anyone with suspected secondary hypoadrenalism e.g. known pituitary disease.
Who / how to refer
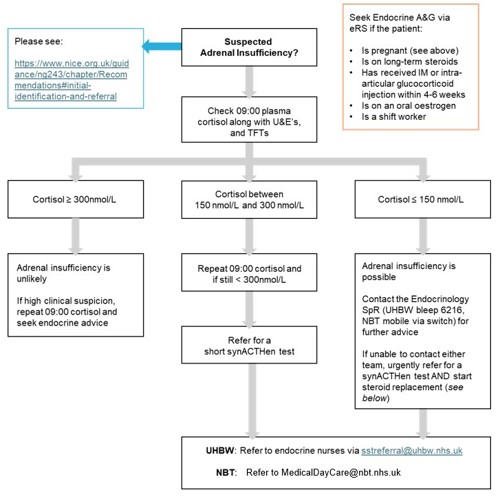
Update on Referral Routes for SST (this is not available via ICE)
The laboratory will advise whether the SST is normal or not.
If SST is abnormal, the patient should be referred to endocrinology via eRS - see Services section below.
If SST is normal then adrenal insufficiency can usually be excluded. Please consider requesting Advice & Guidance for patients with a normal SST and ongoing clinical concern.
All pregnant patients with known adrenal insufficiency or taking supraphysiological doses of corticosteroids should be referred urgently to the Joint Antenatal Endocrine Clinic (JEANC) via the antenatal services where the patient has booked or wishes to deliver.
Management of suspected adrenal insufficiency – starting steroids
- In those with suspected adrenal insufficiency AND a 9am cortisol < 150nmol/L:
- Start steroids whilst waiting for a synacthen test or Endocrine review
- The Endocrine SpR can be contacted for advice - UHBW bleep 6216 OR Endocrine SpR mobile at NBT (via switch)
- Commence
- Hydrocortisone in 3 divided doses: 10mg on waking, 5mg at lunchtime and 5mg in the evening
OR
-
- Prednisolone at a total daily dose of 4mg OD taken on waking (July 25)
Information for those with known adrenal Insufficiency (Sick Day rules)
Information regarding sick day rules can be found here:
Resources
References
(1) Primary Adrenal Insufficiency Guideline Resources | Endocrine Society
(2) SOCIETY FOR ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE: Emergency management of acute adrenal insufficiency (adrenal crisis) in adult patients (2016)
(3) Adrenal insufficiency: identification and management | Guidance | NICE
CKS has advice on when to suspect and how to diagnose Addison's Disease .
Emergency Kits
Emergency kits for people with adrenal insufficiency recommended to avoid hospital admission | NICE
Steroid Emergency Card
NHS England » National Patient Safety Alert – Steroid Emergency Card to support early recognition and treatment of adrenal crisis in adults
Services
Description of service:
• Adrenal Disorders
• Metabolic Bone Disorders
• Pituitary & Hypothalamic
• Thyroid / Parathyroid
Urgent advice pending review or for existing NBT Endocrine patients (if likely to change management within next 72 hours) the team can be contacted via:
Referral: Via e-referral system (eRS)
Description of service:
• Adrenal Disorders
• Metabolic Bone Disorders
• Pituitary & Hypothalamic
• Thyroid / Parathyroid
• Joint Thyroid/Eye Clinic
• Grave's Disease (Thyroid Eye Disease)
Please see the UHBW website for further information on specific clinics.
Urgent advice - ring switchboard and ask to be put through to the diabetes endocrine bleep holder.
Advice & Guidance is also available via eRS
Referral: Via e-referral system (eRS)
Efforts are made to ensure the accuracy and agreement of these guidelines, including any content uploaded, referred to or linked to from the system. However, BNSSG ICB cannot guarantee this. This guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer, in accordance with the mental capacity act, and informed by the summary of product characteristics of any drugs they are considering. Practitioners are required to perform their duties in accordance with the law and their regulators and nothing in this guidance should be interpreted in a way that would be inconsistent with compliance with those duties.
Information provided through Remedy is continually updated so please be aware any printed copies may quickly become out of date.